Beyond the Ache: Expert Solutions for Chronic Pain
Why Understanding Chronic Pain Relief Is Your First Step Forward

Chronic pain relief can feel impossible when you're living with pain that persists for months or even years. But here's what you need to know right away:
Top Chronic Pain Relief Options:
- Medical treatments: NSAIDs, antidepressants, nerve blocks, injections
- Physical therapies: Gentle exercise, swimming, yoga, physical therapy
- Mind-body approaches: CBT, mindfulness meditation, breathing exercises
- Natural therapies: Acupuncture, massage, cryotherapy, red light therapy
- Lifestyle changes: Anti-inflammatory diet, sleep hygiene, stress management
- Self-help strategies: Pacing activities, support groups, distraction techniques
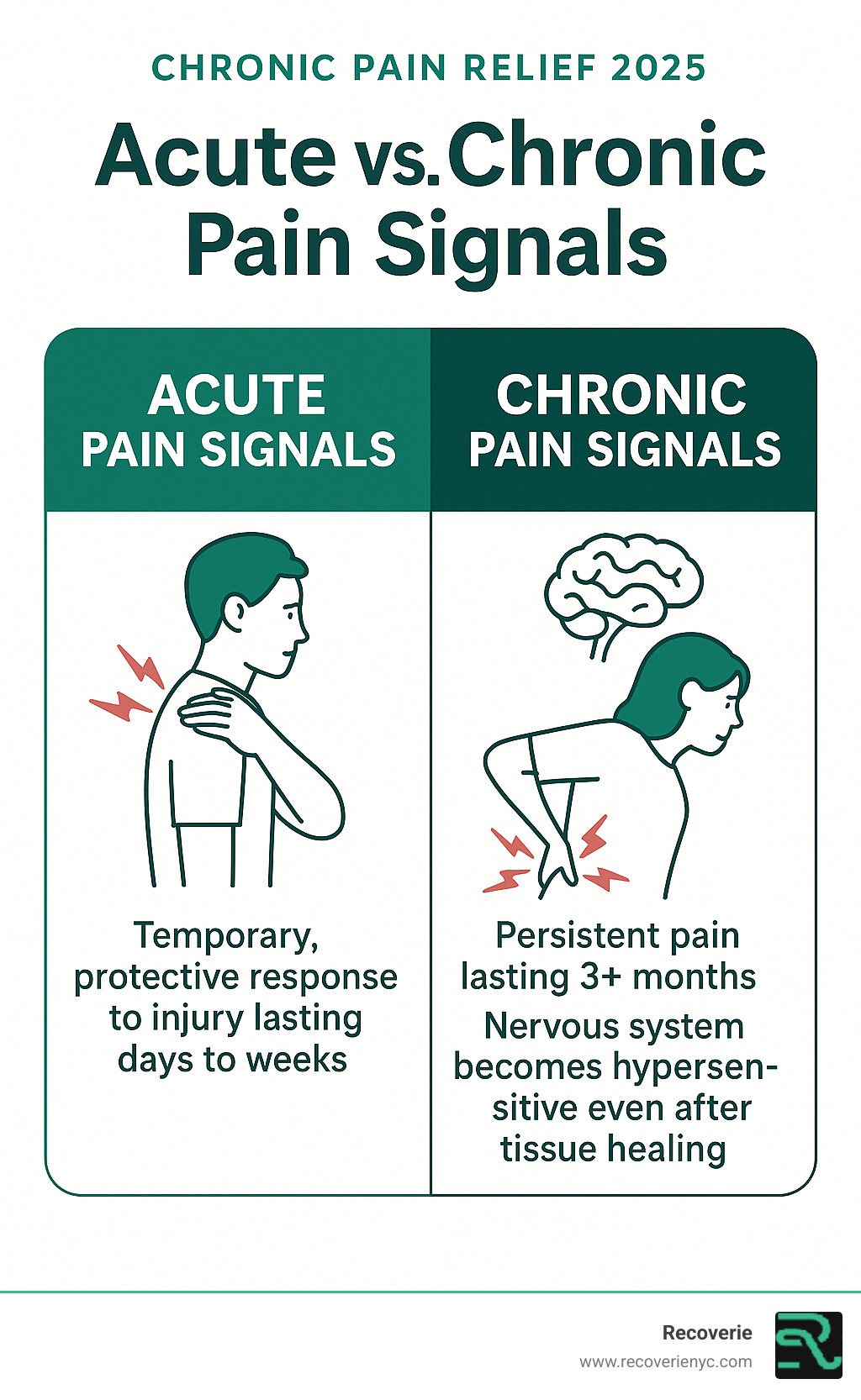
Living with chronic pain means dealing with discomfort that lasts three months or longer - long after your body should have healed. Unlike acute pain that serves as a warning signal, chronic pain often persists without serving any protective purpose.
The numbers tell the story: 3 out of 10 people in the U.S. live with chronic, persistent pain. If you're one of them, you know how it can affect nearly every aspect of your life - from work and relationships to sleep and mental health.
As one Cleveland Clinic expert puts it: "It may feel more like existing with pain than living."
But here's the good news: chronic pain is manageable . While it may not always be curable, effective treatments can help you regain control of your life. The key is understanding that there's no "one-size-fits-all" solution - finding what works for you often requires a personalized approach combining multiple strategies.
Your pain is real, your struggle is valid, and relief is possible.
Understanding the Far-Reaching Impact of Chronic Pain
Living with chronic pain isn't just about physical discomfort; it's a profound experience that can ripple through every aspect of a person's life. When pain becomes a constant companion, it can steal our energy, our joy, and even our sense of self.
Physically, chronic pain can lead to decreased mobility, muscle weakness, and a general decline in physical function. Simple tasks like walking, lifting, or even sitting can become agonizing. This often leads to a vicious cycle: pain causes inactivity, which in turn causes muscles to weaken and joints to stiffen, potentially worsening the pain.
The mental and emotional toll is equally heavy. Imagine constantly battling an invisible foe. This relentless struggle often leads to what experts call the "terrible triad": suffering, sleeplessness, and sadness. Chronic pain can trigger anxiety, depression, and irritability. We might find ourselves withdrawing from social activities, feeling isolated, and struggling to maintain relationships. When pain interferes with work or social life, it can feel like we're "existing with pain rather than living." Our quality of life can diminish significantly, making it hard to pursue hobbies, engage with loved ones, or even care for ourselves.
How Pain Changes the Nervous System
One of the most fascinating and challenging aspects of chronic pain is how it can literally change our nervous system. Unlike acute pain, which is a clear signal that something is wrong (like touching a hot stove), chronic pain often persists long after any initial injury has healed. This is because our nervous system can become hypersensitive, a phenomenon known as "central sensitization."
Think of it like a city with a single highway for pain signals. In chronic pain, that single highway expands into multiple superhighways, making it easier for pain signals to travel and even amplify. Specialized nervous system cells called glia can also contribute to ongoing inflammation, sending constant pain signals even when there's no direct threat. This means the pain we feel is incredibly real, even if there's no obvious physical damage. Pain is a subjective experience, and there's no diagnostic test that can objectively measure someone's pain level. Understanding this neurobiological shift is key to effective chronic pain relief .

Common Conditions Associated with Chronic Pain
Chronic pain isn't a single condition; it's a symptom that can stem from a variety of underlying issues. Many common conditions lead to persistent pain, each with its own unique challenges.
Some of the most prevalent include:
- Arthritis: Affecting over 50 million Americans each year, arthritis causes joint inflammation and stiffness, leading to chronic discomfort.
- Fibromyalgia: A widespread pain condition characterized by muscle pain, fatigue, sleep problems, and mood issues.
- Low-back pain: A significant health problem and one of the most common causes of activity limitation.
- Headaches and migraines: Recurrent, severe headaches can be debilitating and chronic for many individuals.
- Neuropathic pain: This type of pain results from damage or dysfunction of the nervous system itself, often described as burning, tingling, or shooting sensations.
- Myofascial Pain Syndrome: This condition involves chronic pain in the fascia (connective tissue) and muscles.
- Cancer pain: Many people with advanced cancer experience persistent pain as a symptom of their disease or its treatment.
Understanding the specific cause of your chronic pain is an important step in finding the right path to chronic pain relief .
Coping with Chronic Pain (American Psychological Association)
A Holistic Blueprint for Chronic Pain Relief
Given the complex nature of chronic pain, a single solution rarely works for everyone. That's why we advocate for a holistic, multidisciplinary approach. This means assembling a team of healthcare professionals who work together to address all aspects of your pain – physical, mental, and emotional.
There's truly no "one-size-fits-all" for chronic pain relief . What works wonders for one person's low back pain might not touch another's osteoarthritis. Our primary goals in pain management aren't always about eliminating pain entirely (though that's certainly a dream!). More realistically, we aim to reduce pain levels, maximize your function, and significantly improve your quality of life. This personalized approach acknowledges your unique needs and preferences, returning control to you.
Medical Treatments and the Quest for Chronic Pain Relief
When it comes to chronic pain relief , medications often play a role, but it's crucial to understand their benefits and risks. We always balance pain relief with safety.
Over-the-Counter Medications:
- NSAIDs (Nonsteroidal Anti-Inflammatory Drugs): Medications like ibuprofen and naproxen work by blocking enzymes involved in pain and inflammation. They're great for arthritis, sprains, and muscle pain. However, they have a "ceiling effect" – taking more doesn't provide extra relief and can increase side effects like stomach issues or kidney damage.
- Acetaminophen: Known for headache and general pain relief, it's generally safer than NSAIDs for the stomach. But be cautious with dosage; too much can harm the liver and kidneys, especially with alcohol.
Prescription Medications:
- Antidepressants and Anti-Seizure Medications: These might seem surprising, but certain types can effectively quiet pain signals from nerve cells. They're often used for chronic nerve pain, fibromyalgia, and migraines, often at lower doses than those used for depression or seizures.
- Opioids: These mimic our body's natural pain-relieving chemicals. While highly effective for acute pain (like after surgery or a broken bone), their role in long-term chronic pain relief is severely limited and comes with significant risks. Chronic opioid therapy rarely shows more than one-third pain reduction in studies extending beyond 18 months. Risks include tolerance (needing more for the same effect), dependence, addiction, and overdose deaths. We consider them a last resort for chronic pain, and their use requires careful, frequent follow-up with your healthcare provider.
| Medication Type | How It Works | Common Uses | Benefits | Risks/Considerations |
|---|---|---|---|---|
| Non-Opioids (NSAIDs, Acetaminophen) | Modulate pain signals, reduce inflammation. | Headaches, muscle pain, arthritis pain, mild chronic pain. | Readily available, generally safe for short-term use, fewer serious side effects. | Liver/kidney damage (high doses), stomach upset, bleeding risk (NSAIDs), "ceiling effect" (NSAIDs). |
| Antidepressants | Modulate pain signals; affect mood and perception. | Chronic nerve pain, fibromyalgia, chronic low back pain. | Can have various side effects (e.g., dry mouth, blurred vision, weight gain, sexual dysfunction), dosage must be carefully managed. | |
| Opioids | Mimic natural pain relief; bind to pain receptors. | Acute pain (surgery, severe trauma), sometimes for severe chronic pain (last resort). | Rapid relief, effective for severe pain. | High risk of tolerance, dependency, addiction, severe withdrawal, overdose death, constipation, sedation, nausea, respiratory depression. |
| Op Opioid Pain Medications | Bind to opioid receptors in the brain and spinal cord, modulating pain perception. | Moderate to severe chronic pain when other options are insufficient (carefully selected cases). | Can provide significant pain relief when other options fail. | High risk of dependence, addiction, tolerance, withdrawal symptoms, opioid-induced hyperalgesia (OIH), respiratory depression, constipation, nausea, vomiting. Requires strict monitoring and often part of a comprehensive plan. |










